There you are, walking around the house, maybe on your way to get something to eat or to the living room to watch some TV.
All of a sudden, one side of your body goes numb and weak, and you lose your balance, causing you to collapse on the floor.
When you try to call for help, you find that you can’t speak properly with your speech sounding slurred.
You realise that you can’t see properly either, as your vision has become blurry.
And when you look at your face in the mirror, you realise that one side is drooping down, but not the other.
You are most likely experiencing a stroke, the third most common cause of death in Malaysia.
This emergency condition occurs when the brain is deprived of vital oxygen supply, either when a blood clot blocks off a blood vessel supplying the brain (ischaemic stroke) or when one of these blood vessels ruptures and starts bleeding (haemorrhagic stroke).
According to consultant neurologist Dr Kok Chin Yong. your brain cells will start to die within minutes after the stroke hits you – about 2,000,000 cells every minute.
Therefore, you need to get help and go to the nearest hospital’s emergency department as soon as possible.
The good news is that there are immediate treatments that can not only save your life, but also minimise any disability you might have from the stroke.
Ischaemic strokes are the most common type of stroke, comprising three-quarters of all cases.
For this type of stroke, the first and most immediate treatment is the administration of tissue plasminogen activators (tPAs), which help break down blood clots.
Says Dr Kok: “For an ischaemic stroke, the target is to unblock the blood clot as soon as possible.
“We can do this with an intravenous (IV) clot-busting agent called alteplase.
“The current guidelines state a cut-off point of 4.5 hours from the onset of symptoms in order to derive benefit from this treatment.
“Hence, time is brain.”
He notes that alteplase is the only US Food and Drug Administration-approved tPA for acute ischaemic stroke at the moment.
Another treatment available in certain hospitals, he adds, is a clot-removal procedure called mechanical thrombectomy, which is done by an interventional radiologist.
Meanwhile, haemorrhagic strokes are usually treated by the neurosurgeon or interventional radiologist.
Explains consultant neurosurgeon Dr Gerard Arvind Martin: “Choosing whether to take the patient to the operating room or not can depend on various factors, such as age and condition of the patient, the level of consciousness and extent of bleeding, all of which the surgeon takes into consideration before performing surgery.
“In those cases where a subarachnoid haemorrhage has occurred due to a suspected aneurysmal rupture, a further scan called an angiogram will be required to determine precisely the site of bleeding.
“Angiograms can be either via computed tomography (CT) scan or a catheter, which is typically carried out by a radiologist in an angiogram suite.
“Depending on the findings, the surgeon can then elect to operate and clip the ruptured aneurysm, or consider endovascular techniques, which are performed by an interventional radiologist.”
If you are lucky, you would have survived your stroke with no or minor complications and have a quick recovery.
However, many stroke survivors will face long-term disability, which can be physical or cognitive.
For example, patients may experience paralysis of the side affected by the stroke; weak coordination; difficulty in speaking, understanding, reading and writing; and difficulty concentrating.
A stroke patient exercises his muscles with the help of a machine, supervised by a physiotherapist.
 |
Physiotherapy Treatment in Malaysia
https://youtu.be/PYQO3SDe8_w ”
Dr Wong Yee Choon - Mix FM Doctor On Call
How much you know about Stroke? Stroke is an emergency, every minute counts – Act F.A.S.T.
Listen to Dr Wong Yee Choon, consultant Neurologist being interviewed by Mix FM - Doctor On Call.
Topic: Stroke - Act F.A.S.T
https://www.facebook.com/PantaiHospitalPenang/videos/1806467726066530/
https://youtu.be/PYQO3SDe8_w ”
Dr Wong Yee Choon - Mix FM Doctor On Call
How much you know about Stroke? Stroke is an emergency, every minute counts – Act F.A.S.T.
Listen to Dr Wong Yee Choon, consultant Neurologist being interviewed by Mix FM - Doctor On Call.
Topic: Stroke - Act F.A.S.T
https://www.facebook.com/PantaiHospitalPenang/videos/1806467726066530/
Says Dr Kok: “This is an area that is often given less attention, when in fact, to me, it is equally important as the acute treatment for stroke.
“A good rehabilitation programme improves disability and prevents complications.”
According to Sunway Medical Centre Velocity Rehabilitation Centre head Maxim Chea, stroke rehabilitation has to be individualised to the patient as it depends on the part of the body or type of ability affected by the stroke.
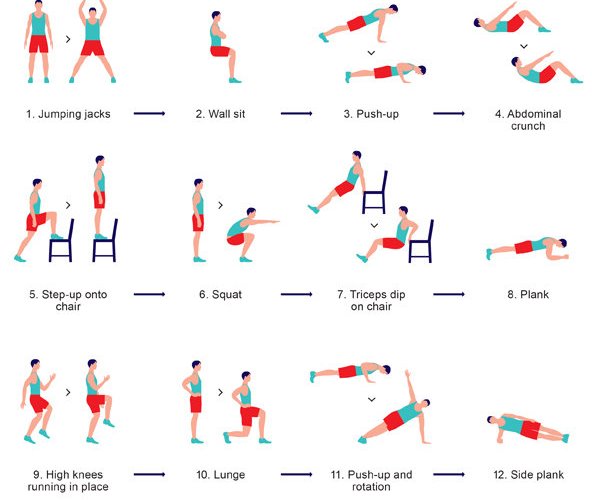
He explains that there are three main types of rehabilitation therapy: physical therapy, technology-assisted physical therapy (e.g. functional electrical stimulation and virtual reality), and cognitive and emotional therapy.
Visual rehabilitation is also available for those whose vision is affected by stroke.
For example, consultant neuro-ophthalmologist Dr Lakana Kumar shares that “Double vision and peripheral loss of vision can be treated with prisms incorporated into glasses for patients to wear.”
Rehabilitation is usually carried out by a team consisting of physiotherapists, occupational therapists, speech therapists, and dieticians/nutritionists, among others.
In addition to physical and cognitive problems, patients might easily become depressed, overly anxious and panic easily.
Says consultant psychiatrist Dr Lim Wai Jenn: “Stroke survivors are at significantly higher risk for neuropsychiatric conditions such as post-stroke depression (one in three patients), anxiety (one in four patients), and other changes in personality and behaviour.
“These conditions impede the rehabilitation process and degree of recovery in post-stroke patients.
“They also significantly impact the patients’ long-term functioning and quality of life, and can even lead to higher mortality rates.
“Early psychiatric assessment and intervention is essential.”
She notes that caregivers also need support and psychoeducation on how best to support patients in regaining function.
While being affected by a stroke is a frightening event, rest assured that there are treatments and therapies available to help you manage this condition – just remember that you need to seek medical help as soon as possible.
By TAN SHIOW CHIN This article is courtesy of Velocity Neurocentre, Sunway Medical Centre Velocity.
Source link
7 stages of stroke recovery: Why home rehabilitation is important

A CT scan of a stroke patient’s brain, showing the affected area of their brain (in violet). The affected area will determine the type and extent of disabilities the patient will have. — Schering AG
By Matthew Teo Yong Chang
Stroke or a cerebral vascular accident (CVA) was the third leading cause of death in Malaysia in 2018, according to the Department of Statistics. The department reported that stroke caused 7.1% of all deaths in the country. However, two-thirds of those who have a stroke actually survive and will require rehabilitation.
The objectives of rehabilitation are to help survivors become as independent as possible and to attain the best possible quality of life. It is crucial as stroke survivors can lose the function of their affected limbs without rehabilitation, something we have observed in real life.
Even though the function of a stroke survivor’s affected limbs may seem lost after the stroke, our brain possesses a trait called neuroplasticity that can help the survivor regain the limb’s function.
Neuroplasticity enables the unaffected nerve cells (neurons) around the affected area of the brain to rewire and create new pathways around the affected area through repetition of physical and mental training, as well as regulated emotional feedback.
However, the extent for neuroplasticity varies in each individual. So, even though rehabilitation does not “cure” the effects of stroke, in that it does not reverse brain damage, rehabilitation can considerably help survivors achieve the best possible outcome in the long run.
Levels of disability
Rehabilitation, rehab, stroke, physiotherapy, activities of daily living, occupational therapy, Star2.com Rehabilitation is aimed at regaining practical function for the patient, like opening a door latch, turning a tap or pushing a switch.
Strokes happen when a blood clot or bleeding (haemorrhage) restricts the blood supply to the brain, resulting in the brain being deprived of oxygen, which leads to the death of brain cells.
Usually, it is only one part of the brain that is damaged and this affects the type and degree of disability the survivor will experience. This also influences how much rehabilitation can help the survivor.
Generally, stroke can cause five types of disabilities:
• Paralysis, or problems controlling voluntary movement
• Disturbance of the senses, including pain
• Problems using or understanding language
• Problems with thinking and memory
• Emotional disturbances
It is also imperative to know the severity of the stroke before deciding on the rehabilitation plan. There are seven recognised stages of stroke recovery through which most survivors progress through:
• Stage 1 – Flaccidity: No voluntary movement is observed.
• Stage 2 – Spasticity appears: Spasticity refers to the continuous contraction of muscles, which interferes with normal movement, speech and gait, and causes the arm or leg to make small involuntary jerky movements.
• Stage 3 – Increased spasticity: The e arm or leg becomes more spastic, and the muscles feel stiff and tight against external resistance.
• Stage 4– Decreased spasticity: Spasticity of the arm or leg decreases and the limb begins to move more easily.
• Stage 5 – Complex movement combinations: The movement of the limbs start becoming more coordinated and full movement begins to return.
• Stage 6 – Spasticity disappears: Muscle spasticity disappears and isolated joint movements are voluntary; however, spasticity may return if the patient is tired.
• Stage 7 – Normal function returns: Movements return to normal.
Each stage requires different types of approaches and exercises for rehabilitation.
Home rehab

The rehabilitation programme for stroke survivors involves a multidisciplinary healthcare team consisting of a rehabilitation physician, nurses, occupational therapist, physiotherapist, speech therapist, dietitian and clinical psychologist.
However, the most important members of the team are the patient and their caregivers. This is as rehabilitation should be done daily at home, not just during therapy appointments.
Battling stroke disabilities is not as simple a remedy as taking a pill from the doctor or attending a session with the therapist for an hour a week. It requires compliance to medication and the continuous effort to practice the therapies repetitively with strong determination!
Contrary to common belief, stroke rehabilitation can be offered in any setting without sophisticated equipment or technology.
The American Heart Association recommends that stroke survivors perform aerobic exercises three to seven days per week, as well as strengthening, flexibility and neuromuscular exercises two to three days a week, for the rest of their life.
Training at home, in a familiar environment, by adapting and using utensils or tools at home is more meaningful than the therapeutic remedial therapy received at institutionalised centres.
For instance, toilet training at a hospital ward is not as useful as toilet training in your own home, as you will eventually be going home and using that toilet, rather than the hospital’s toilet.
After all, the ultimate goal of rehabilitation is to promote optimal functional independence in the survivor’s own living environment.
Besides, providing therapy in the home environment supports continuity of care, provides a relevant environment for daily function, and encourages patients to develop problem-solving skills.
Some of the other benefits of home rehabilitation for stroke include:
• Early discharge from the hospital to return to the comfort of your own home.
• Avoiding hospital-acquired pneumonia and other illnesses due to a shorter stay.
• Reducing the cost of care.
• Preventing deterioration and promoting health through physical activity.
• Preventing falls, which are common among older patients and can cause additional long-term disability.
Barriers to home rehab
The main barriers towards rehabilitation in stroke are a lack of motivation and apathy towards recovery. Most stroke survivors stop coming for their treatment regime after a period of rehabilitation because they do not see any significant improvement.
Over a period of time, they will begin to learn helplessness and compensate themselves – mostly incorrectly – for their abnormal postures and movement, leading to non-compliance in rehabilitation.
Poor awareness among the public about the different roles of the different therapists in stroke rehabilitation could also be another barrier in rehabilitation.
In addition, the lack of trained therapists in Malaysia for stroke rehabilitation is also another factor, as it contributes to increased cost of hiring in-house therapists for home rehabilitation due to their scarcity.
Matthew Teo Yong Chang is a lecturer in the School of Occupational Therapy at the Perdana University Graduate School of Medicine. This article is courtesy of Perdana University. For more information, email starhealth@thestar.com.my. The information provided is for educational and communication purposes only and it should not be construed as personal medical advice. Information published in this article is not intended to replace, supplant or augment a consultation with a health professional regarding the reader’s own medical care. The Star disclaims all responsibility for any losses, damage to property or personal injury suffered directly or indirectly from reliance on such information.
Stroke Hand Exercises: For every stage of recovery
https://youtu.be/gDxyQGyOx_0
Source link
Post-Stroke Exercises (Part 1: Upper Limb)
A physiotherapist explains safe lower limb exercises for stroke patients This video is brought to you by Singapore General Hospital.
https://youtu.be/3GbpbuwcWDk
Post-Stroke Exercises (Part 2: Lower Limb)
https://youtu.be/BM0P-iLSlbs
Stroke Exercises for Arm & Hand with Little to No Strength-for Home
"Famous" Physical Therapists Bob Schrupp & Brad Heineck demonstrate stroke exercises you can do in your own home for the arm and hand that has little to no strength.https://youtu.be/DoR9H9zuJPY
Stretches For Hand Spasticity - Best Stroke Recovery Hand Exercises
https://youtu.be/dBWRuy_hdoc
Best Stroke Recovery Hand Exercises - Stage 1
https://youtu.be/ZKR1nOtCNKU
Best Stroke Recovery Hand Exercises - Stage 2
https://youtu.be/oZrQU72dGO0
Best Stroke Recovery Hand Exercises - Stage 3
https://youtu.be/zpseq7i4_7ATaking Care Of Your Gut Is Key To Stronger Immunity
Taking Care Of Your Gut Is Key To Stronger Immunity | The Star
Others: One minute exercise cures: https://mp.weixin.qq.com/s/
Related posts:
Exercises for Stroke Patients
- Upper Limb Exercises
Covid-19 Affecting many organs in our body: road to recovery to gain Strength and immunity
COVID-19's neurological symptoms; the next hotspots; COVID modelling
COVID-19 can affect the brain. How it happens and what to watch for.
⇒ Explore: COVID-19
Recognition and Management of Stroke
Rehabilitation key to improving health
DAEHAN Rehabilitation Hospital Putrajaya offers customised rehabilitation services that focus on intensity and discipline to give patients with neurological and orthopaedic disabilities optimal results.
Strokes and other neurological disabilities often leave individuals with lasting and damaging effects that can greatly impede their daily functions.
This brings to light the need to raise awareness on the crucial and beneficial role rehabilitation can play in the lives of such patients.
According to Dr Fazah Akhtar, studies have shown that early and high-intensity rehabilitation has given patients better outcomes.
“Certain neurological conditions such as strokes and traumatic brain injury have a window period of best recovery after the event,” said Dr Fazah.
“If an individual were to undergo high-intensity inpatient rehabilitation in a specialised hospital or unit, the recovery and functional outcomes of the patient have shown to be better than those who do not receive such treatment.”
Understanding this approach, Daehan Rehabilitation Hospital Putrajaya offers South Koreanstyled rehabilitation services in which they are on a one-on-one basis and are personalised to specifically match the needs of the individual.
Besides stroke patients, they also manage cases of traumatic brain injuries, hypoxic brain injuries, brain tumours, spinal cord injuries, musculoskeletal conditions and other complex conditions that require multidisciplinary rehabilitation.
With an emphasis on intensity and discipline, the inpatient rehabilitation programmes are planned and targeted for a duration of three months with extensions as needed.
A programme’s daily schedule usually features several rehabilitation sessions, starting at 9am and end at 5pm.
In addition, parts of the programme are practised in open and spacious therapy areas such as the gymnasium to enhance engagement and social interactions between patients.
This forms a support group system and such peer encouragement has seen a positive impact on the programme, says Dr Fazah.
All this is further augmented by technological advancements such as gait robotics, computerbased therapy, individualised hydrotherapy, and anti-gravity treadmills.
Their full list of therapy programmes includes physiotherapy, occupational therapy, functional electrical stimulation (FES), pain therapy, speech therapy, dysphagia rehabilitation, computerised cognitive function therapy, activities for daily living (ADL) training, return to work training, pulmonary rehabilitation, machine treatment, gait training with special equipment, robot-assisted gait trainer, hydrotherapy treadmill, and anti-gravity treadmill.
Meanwhile, their facilities and services include an emergency department, room and board, imaging department, specialist clinic, daycare service, inpatient and outpatient services, and outdoor therapy.
While Daehan Rehabilitation Hospital Putrajaya only offers its services to adults at this point, there are plans to expand to paediatrics rehabilitation soon.
Certain neurological conditions such as strokes and traumatic brain injury have a window period of best recovery after the event.
-Dr Fazah Akhtar
Others:
SBS - Sure Boh Singapore
·Founding Father Lee Kuan Yew's famous quote:
Founding Father Lee Kuan Yew's famous quote. I'm surprised it took them 65 minutes. I would have apologised straight away after he says "STOP IT!